Day 1 :
- Surgical Case Reports
Location: Sydney, Australia
Session Introduction
Jacqueline Hawthorne
Hunter New England Health, Australia
Title: Appendicitis in an Incarcerated Femoral Hernia: a case of De Garengeot Hernia

Biography:
Jacqueline is currently working at Hunter New England Health.
Abstract:
Introduction
The finding of an incarcerated femoral hernia containing the appendix is a rare phenomona occuring in less than 1% of fermoral hernias. 0.08-0.13% of femoral hernias contain an incarcerated acute appendicitis. These are known as De Garengeot hernias. Often diagnosis occurs at operation due to lack of symptoms of acute appendicitis (1).
Presentation of Case
68 year old female presented with painful right groin lump for several weeks. She did not have any obstructive symptoms. Ultrasound reveled an incarcerated femoral hernia, CT scan confirmed righ femoral hernia comntaining a loop of small bowel. Laporatory findings showed a normal white cell count and c-reactive protein. A diagnostic laparoscopy was performed identifying a right femoral hernia containing the appendix. A sub-total laparoscopic appendicectomy was performed as well as an open right femoral hernia repair, through which the tip of the appendix was removed. Histopathology confirmed acute appendicitis. She recovered well.
Discussion
Pre-operative diagnosis is extremely difficult in De Garengeot hernia. Radiological studies are usually non-specific, or may identify a femoral hernia with incarceration, despite a lack of symptoms suggestive of small bowel obstruction. Laporatory results are also non-specific. In hindsight, the suggestion of small bowel in the femoral hernia with a lack of symptoms was the key to the diagnosis of De Garengeot hernia. It is unclear whether the appendix became inflammed due to being inside the femoral hernia or whether the patient developed acute appendicitis which then migrated into the femoral hernia.
Veral Vishnoi
John Hunter Hospital, Australia
Title: Small bowel obstruction from metastatic mesenteric/omental infiltration from a cutaneous squamous cell carcinoma: A rare presentation

Biography:
Veral Vishnoi graduated with a Bachelor of Medicine, Bachelor of Surgery with Honours from James Cook University in Queensland, Australia. He is currently working part time as a surgical registrar at the John Hunter Hospital in Newcastle whilst completing his PhD with the university of Newcastle in New South Wales, Australia. His research interests lies in colorectal surgery in particular diverticular disease.
Abstract:
We present a 57-year-old male with known metastatic cutaneous squamous cell carcinoma (SCC) with an unknown primary presenting with a small bowel obstruction. Malignancies of the small bowel are rarely primary, but rather dominated by metastatic melanoma followed by metastatic adenocarcinoma from the pancreas, colon or stomach. Metastatic cutaneous SCC (although rare) travels to lymph nodes, brain, bone, lung and skin, very rarely to the gastrointestinal tract. Our patient had been on palliative chemotherapy when he presented with a one week history of nausea, progressing to faecalent vomiting, abdominal distension and obstipation. A computed tomography scan demonstrated significant stranding around the omentum and mesenteric fat with a small cystic mesenteric mass with a resultant small bowel obstruction. Given that patients advanced disease a conservative approach was taken with gastric decompression via a nasogastric tube and intravenous fluid resuscitation. A radiological guided fine needle aspiration of the mass was performed, confirming cutaneous SCC. To the best of our knowledge this is a very rare occurrence.
Melody Sutedja
Mariano Marcos Memorial Hospital and Medical Center, Phlippines
Title: Mayer-rokitansky-kuster-hauser syndrome with hyperandrogenemia: a rare case of mullerian dysgenesis

Biography:
Melody Nethania Sutedja has completed her Medical School at the age of 23 years from Soochow University in Suzhou, China and currently doing her residency in Mariano Marcos Memorial Hospital and Medical Center in Batac, Philippines. She is in her third year of recidency of OBGYNE. She has published her interesting case In Manila.
Abstract:
Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome with hyperandrogenism is a spectrum of Müllerian duct anomalies characterized by congenital aplasia of the uterus and of the upper part (2/3) of the vagina, in young women presenting infrequently with high level of testosterone. The ovaries and fallopian tubes are present. It is one of the most common causes of primary amenorrhea and affects at least 1 out of 4500 women however there only 4 cases were reported of MRKH syndrome associated with hyperandrogenemia in literature. The MRKH syndrome usually remains undetected up until the patient complains with primary amenorrhea regardless of normal development of secondary sexual physical characteristics. We report a case of MRKH syndrome with hyperandrogenism in a 21-year-old female who presented with primary amenorrhea, Physical examination include Tanner stage 5 breasts, Pubic hair stage IV with absence of cervix, short vaginal canal and no clitoromegaly. Transvaginal ultrasound revealed an infantile uterus while MRI shows small uterus with inactive endometrium and incidental findings of Tarlov cyst. Counseling, assurance and supportive psychotherapy were given to the patient. Follicle stimulating hormone, chest X-ray, 75 gram oral glucose tolerance test, BUN, creatinine, audiogram and electrocardiogram results were all within normal ranges. Chromosomal analysis was 46 XX karyotype. Serum testosterone was markedly elevated at 11.1 nmol/L, above the normal values for both male and female.

Biography:
Michael Ruyssers is currently a surgical resident at the Free University of Brussels in Belgium. During the completion of his medical studies at the Univerisity of Antwerp, from 2007 until 2014, he realized that he wanted to become a surgeon. Now he is fulfilling his 4th year of surgical training in general surgery with a strong interest in abdominal surgery. The first two years of his training were in the University Hospital of Brussels where he mostly learned the basics of surgical care and learned to functionate independantly on the ward and the emergency unit. During this period he also passed his exam in Advanced Trauma Life Support. In the last two years he worked in the Acadamic Hospital Saint Dimpna in Geel. Here he really started to develop his surgical skills, especially in laparoscopy, and created independence in the theatre.
Abstract:
Ho Peiying Audrey
University College Dublin
Title: Case Study in a lady with extensive venous thrombosis

Biography:
Audrey graduated from University College Dublin in 2017 and is currently working in Singapore.
Abstract:
32 year old lady presented with dizziness, 1 week history of peri-umbilical abdominal pain and back pain not associated with recent trauma. It was found that she had symptomatic anemia with Hb 4.4. CTAP showed thrombosis of the right, proximal left and main portal veins, splenic, superior mesenteric veins and the right renal vein extending to the intrahepatic inferior vena cava. Fibroid measuring 9.5 x 8.5 x 8.0 cm was the likely cause of menorrhagia leading to her anemia. She was extensively worked up for auto-immune disease markers eg. Lupus anticoagulant, ANA, anti-cardiolipin, anti-b2, all of which were negative. Coagulation panel markers were slight deranged, with APTT 40.7, PT 15.3. After transfusion with 3 pints to reach a post-transfusion Hb level of 7.9, she was started on clexane and bridged to warfarin, for at least 6 months of anticoagulation with haematology input.
Tiffany L Gould
University of Newcastle, Australia
Title: Spontaneous non-occlusive isolated caecal necrosis - an unusual cause of right iliac fossa pain

Biography:
Tiffany completed a Bachelor of Medicine from the Unviversity of Newcastle, awarded with Distinction in 2015. She has completed further studies in Advanced Surgical Anatomy, as well as a Diploma of Science and a Master of Traumatology awarded with Distinction in 2017. Tiffany is works as a Clinical Teaching Fellow with the University of Newcastle, a surgical registrar in Hunter New England Health and has commenced a research higher degree in the field of Colorectal Surgery and Preventative Medicine.
Abstract:
Abdominal pain is a common clinical presentation particularly in the elderly population and presents a wide range of differential diagnosis. This case reviews an 86-year-old female
with a medical history of hypertension, cholecystectomy, and reflux who presented with lower right sided abdominal pain, nausea and hot and cold flushes. She had opened her bowel the day of presentation, which she stated was normal. On examination, she was in sinus rhythm with a blood pressure of 130/90. She was clinically dehydrated with dry mucus membranes. Her cardiac and respiratory examination were normal. Her abdominal examination revealed a mass in the right lower quadrant that was tender, with local peritonism, guarding and rebound tenderness. The patient was treated with analgesia, intravenous fluid and remained nil by mouth. A CT scan was performed which revealed a mass within the caecum suggestive of a colorectal carcinoma. The patient subsequently underwent a right hemicolectomy, Histological assessment demonstrated a case of acute non-occlusive spontaneous ischaemic colitis. Ischaemic colitis usually results from atherosclerosis and low blood flow. Ischemia of the colon usually affects the left side, however it can also occur anywhere within the colon. Spontaneous non-occlusive ischemic colitis involving the caecum alone is rare, following hemocolectomy the histopathology of the caecal mass revealed a localised area of ischaemic necrosis. There was no evidence of malignancy, vasculitis or embolus identified and there was no significant atherosclerosis. The final diagnosis of this case was spontaneous non-occlusive isolated caecal necrosis.
- Case Reports on Internal Medicine
Location: Sydney, Australia
Session Introduction
Thitinun Anusornvongchai
Diabetes association of Thailand
Title: Rare neuroendocrine tumor secreting vasoactive intestinal peptide with multiple endocrine neoplasia 1: Case report

Biography:
Thitinun graduated and trained in internal medicine from Chulalongkorn university of Thailand. She is a trained endocrinology from department of medical service thailand. Now she is an endocrinologist in lerdsin hospital, Bangkok, Thailand. She is a clinical doctor and also interested in basic research. She also studied about ER stress and saturated fatty acid in Tokyo, Japan (2014-2016). She is currently working on the factors of fracture and osteoporosis, Refracture prevention program. She ia a committee member of diabetes association of Thailand
Abstract:
Objective: Neuroendocrine tumor secreting vasoactive intestinal polypeptide (VIPoma) is rare endocrine tumor.
Materials and Methods: Genomic DNA was extracted from blood leukocyte of the patient using Qiagen’s Blood DNA extraction kit. Genotyping was performed using polymerase chain reaction (PCR) - direct nucleotide sequencing method.
Results: We report case of neuroendocrine tumor secretes vasoactive intestinal polypeptide (VIP) in a 42-year-old Thai female who presented with chronic watery diarrhea and hypokalemic metabolic acidosis for 1 year. The stool was watery, yellow color, non-bloody with volume of about 300 ml each time. Blood for vasoactive intestinal polypeptide level was 360 pg/mL (normal < 75). The computated tomography revealed mass at uncinate process of pancreatic head in parallel with increased tracer uptake at same are by octreotide scan. The study detected 2 variants, the c541 variant has been reported as a genetic polymorphism by Marini F 2008, the most likely disease-causing mutation was Cys409STOP (Cysteine was substituted by STOP codon). Intraoperative finding was presented a 3.5-centimeters light tan round mass at the head of pancreas. Finally, this case went on operation with pyloric preserving pancreatoduodenectomy. During post-operative period, the patient had no serious complication.
Conclusion: Multiple endocrine neoplasia type 1 (MEN1) is rare genetic disorders of multiple endocrine tumors that encoded by MEN1 gene in human. Even though majority of MEN1 are benign and produce endocrine hormones but some are aggressive and presenting with metastatic tumors such as VIPoma.
Surgical resection is gold standard treatment of neuroendocrine tumor. Further studies in parents and siblings are suggested.
Madeline Kirby
American University of The Caribbean School of Medicine, USA
Title: How clinical presentations can delay diagnosis

Biography:
Coming Soon..
Abstract:
Acute promyelocytic leukemia is a rare form of acute myeloid leukemia, representing 5-10% of adult cases of AML. There are an estimated 600-800 newly diagnosed cases in the US every year. It is most commonly taught in medical schools that the presenting symptoms of APML are symptoms of coagulopathy; thrombocytopenia, petechiae, bleeding from the gums. The most severe presentation of APML is of disseminated intravascular coagulation. It is critical to diagnose APML as soon as possible as a delay in diagnosis can lead to severe consequences of bleeding, DIC and mortality. The coagulopathy associated with APML is believed to be due to an activation of protease activity as well as increased fibrinolysis. However, a pro-thrombotic state is also associated with APML although this is exceedingly rare and rarely described in case reports. It is critical to diagnose APML as soon as possible as a delay in diagnosis can lead to severe consequences of bleeding, DIC and mortality. This case report will discuss an acute case of APML diagnosed after presentation with acute ischemic stroke.
- Case Reports on oncology & Cancer
Location: Sydney, Australia
- Case Reports on Cardiology
Location: Sydney, Australia
Session Introduction
DURAID AL-MIDFAI
Fuwai Central China Cardiovascular Hospital, China
Title: Significant genetic association of a functional TFPI variant with circulating fibrinogen levels and coronary artery disease

Biography:
Duraid Al-Midfai considering the cardiovascular major for various reasons. Since I he was a child, he has been fascinated by the world around himself. When he traveled to China and Middle East, the conservation efforts of these two countries interested him and he knew that he wanted to do something related to the CAD disease in Genetics filed. He is currently a member of Fuwai Central China Cardiovascular Hospital As a post doctoral research in the cardio surgery department-in patient building as well as his work also collaborated with Henan Hospital in the Research Center building, which is a Big and famous hospital in central of china for cardiovascular disease treatment.
A long-term goal of him, his goals is to one day manage and discover a novel genes associated with various diseases in human genome. Moreover, he is also curious to learn more about any medical field that is somehow related to genetics research.
Abstract:
The tissue factor pathway inhibitor (TFPI) gene encodes a protease inhibitor with a major role in regulation of blood coagulation. In this project, we performed a large population-based study with 2,313 study subjects for which blood coagulation data are available, including the Fg level, the PT level, the APTT level and the TT level. We selected a functional variant in the promoter of TFPI, rs10931292, which was found to reduce the transcription of TFPI and genotype it in the 2,313 study subjects using the TaqMan assay. We carried out the linear regression analysis under three different genetic models, including an additive model, an autosomal dominant model or an autosomal recessive model, for the genotyping data. Our analysis identified significant association of TFPI variant rs10931292 with increased plasma Fg levels (P=0.017 under a recessive model), but not with PT, APTT or TT (P>0.05). To the best of our knowledge, this is the first time to show that a TFPI variant is significantly associated with plasma Fg levels. These data identify a novel genetic variant for Fg levels and contributes importantly to the elucidation of the genetic basis and biological pathways for plasma Fg levels. An increased plasma Fg level is a well-established risk factor for cardiovascular disease. Therefore, we determined whether TFPI SNP rs10931292 was also associated with risk of CAD. Using a large case control association study population with 4,479 CAD patients and 3,628 controls, we identified significant association between TFPI SNP rs10931292 and CAD under a recessive genetic model (OR = 1.23, P = 0.005). Individuals with the GG/CC genotype had a significantly increased risk of CAD (OR = 1.23, P = 0.005). These data identify a new genetic variant that increases risk of CAD and contributes importantly to the elucidation of the genetic basis and biological pathways for the pathogenesis of CAD.
Image
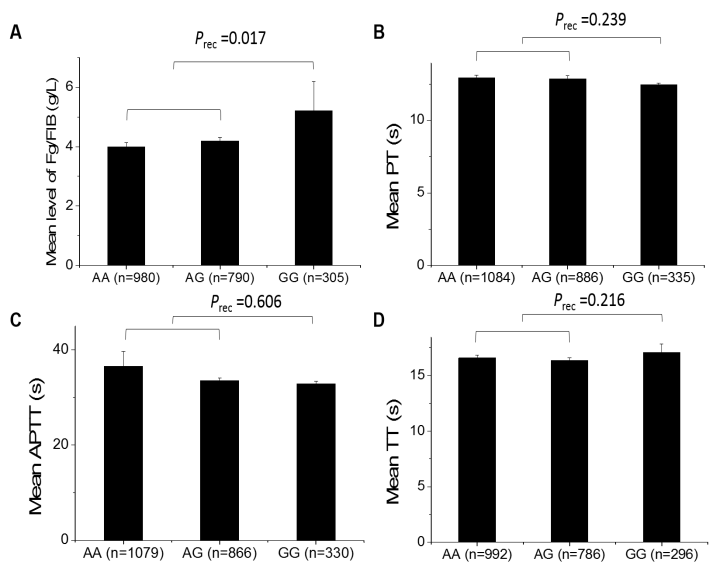
Figure 2.1 Analysis of association of TFPI SNP rs10931292 and coagulation indicators. (A) Fibrinogen levels (Fg/FIB). Mean fibrinogen levels for different genotypes: NAA=980 subjects, 3.99 ± 0.15 g/L; NAG=790 subjects, 4.18 ± 0.14 g/L; NGG=305 subjects, 5.21 ± 0.97 g/L. (B) PPT. Mean PPT for different genotypes: NAA=1084 subjects, 12.92 ± 0.20 s; NAG=886 subjects, 12.86 ± 0.23 s; NGG=335 subjects, 12.46 ± 0.10 s. (C) APTT. Mean APTT for different genotypes: NAA=1079 subjects, 36.52 ± 3.14 s; NAG=866 subjects, 33.59 ± 0.46 s; NGG=330 subjects, 32.89 ± 0.49 s. (D) TT. Mean TT for different genotypes: NAA=992 subjects, 16.58 ± 0.24 s; NAG=786 subjects, 16.34 ± 0.28 s; NGG=296 subjects, 17.08 ± 0.76 s. Prec, P value after adjustment with age and gender under a recessive model.
Jasper Pablo
Philippine Heart Center, Philippines
Title: A rare case of syphilitic aortic aneurysm in the era of modern antibiotics

Biography:
Jasper Pablo had his expertise in training at 2 of the best institutions in the Philippines. He is currently undergoing Fellowship training at the Philippine Heart Center in Philippines. His paper enlightens everyone that Syphilis is still a concern in developing countries.
Abstract:
INTRODUCTION: In this age of medicine, most abdominal aortic aneurysms are of atherosclerotic in origin. Cardiovascular syphilis is a tertiary form of syphilis occurring in 10% of infected patients. It can affect the heart, great vessels and medium-sized arteries. Aortic involvement can present as uncomplicated aortitis, coronary ostial stenosis, aortic regurgitation, and aortic aneurysm. If left untreated, the mortality rate at 1 year can reach 80% due to the high rate of rupture of these aneurysms.
CASE: A 65-year old male, who came in due to chest pain. CT aortogram revealed a fusiform infrarenal aneurysm. Coronary angiogram was done which revealed 3-vessel coronary artery disease. He was tested positive for syphilis and was treated with Penicillin. A dilemma sets in if CABG and open repair of the infrarenal aneurysm is possible. A Thallium scan showed no inducible ischemia, hence, CABG was postponed. An open repair via retroperitoneal approach was done. Histopathologic examination of the aneurysm was consistent with syphilitic aneurysm. He was discharged apparently well until his most recent follow-up.
CONCLUSION: Tertiary syphilis, though a rare disease in this age of antibiotics, is a re-emerging cause of aneurysm and should be considered in patients with risk factors.
- Case Reports on Pulmonology
Location: Sydney, Australia
Session Introduction
Rittigorn Apinhapanit
Lerdsin Hospital, Thailand
Title: Hodgkin’s lymphoma presented with endotracheal and endobronchial mass – a rare case report

Biography:
Rittigorn is a Medical doctor, faculty of medicine at Rangsit university. He is also working as a Resident in Internal Medicine, Department of Medicine at Lerdsin-Rajavithi hospital. He has Fellowship in pulmonary and critical care medicine, Department of Medicine at Ramathibodhi Hospital, Thailand and now is an Attending staff of medicine and ICU as a Chest medicine specialist, Department of Medicine, Lerdsin Hospital, Bangkok, Thailand.
Abstract:
A 20 year-old male presented with two months history of progressive dyspnea with night sweat and dry cough. He was admitted at Lerdsin hospital due to fever for 2 weeks and increase productive sputum. Initial investigation showed mild leukocytosis, chest radiograph showed right lower lobe consolidation and sputum AFB was negative for 3 days. He was clinically diagnosed community acquired pneumonia. After 10 days of intravenous ceftriaxone and oral azithromycin. His fever and sputum were improved but he still had dyspnea especially on lying position. Physical examination revealed central rhonchi after force inspiration suspected of endobronchial lesion. Computer tomography of chest was performed and revealed large endotracheal mass extend to right main bronchus and bronchus intermedius causing obstructive pneumonia at right middle lobe. Flexible bronchoscopy with cryotherapy and endobronchial mass removal was performed, showed intraluminal lobulated endobronchial mass at right anterior portion of the trachea extend to proximal right main bronchus. The pathology revealed positive hematologic malignancy along with positive CD3 (diffuse presence of T-cell) and CD 20 (patchy density). Hodgkin’s lymphoma was diagnosed and then his was sent to hematologist for aggressive chemotherapy. This case is the rare presentation of Hodgkin’s lymphoma because almost cases of lymphoma-related endobronchial mass usually presented in non-Hodgkin’s disease. The hallmark of diagnosis of large endobronchial lesion are presented of dyspnea on lying position (mass effect) and physical examination shown central rhonchi after force inspiration which are helpful for general physician to prevent missing some early-curable disease like this case.
Mandeep
Shri Guru Ram Rai Institute of Science and Technology, India
Title: Drug induced pemphigus vulgaris: case report

Biography:
Abstract:
Pemphigus Vulgaris (PV) is an autoimmune disease affecting oral mucosal membrane and skin. This disease shows a characteristic feature of intraepithelial blistering of both the membranes. A 32yr old female patient was admitted into the hospital with the chief complaints of skin allergy, abdominal pain and difficulty in eating and swallowing. For diagnosis physical examination and immune fluorescence tests were performed. The treatment was given Tab. Solumedrol 8mg OD, Tab. Cetrizine5mg HS, Cap Pantop 20mg OD, Tab. R CINEX 250/300mg OD,Tab. Combutol 800mg OD, Tab Febuzade 40mg BD, Tab. Lesuride 25mg BD, Tab.Omnacortil 20mg ABF OD. Emoderate lotion + Tenovate ointment. Early the diagnosis and treatment less is the suffering to the patient.
- Case Reports on oncology & Cancer
Location: Sydney, Australia
Session Introduction
Battulga Purevdorj
Mongolian National University of Medical Sciences, Mongolia
Title: Case report: mesenteric lymphangioma

Biography:
MNUMS, School of Medicine, Department of Oncology – Hematology
Abstract:
Introduction:
Mesenteric lymphangioma is defined as a cystic lesion located between the leaflets of the mesentery from the duodenum to the rectum, being most commonly found in ileum level. The etiology is unclear. The preoperative diagnosis is often difficult to investigate, because the clinical manifestations are variable mostly it has silent clinical course. Lymphangiomas are benign tumors, probably congenital, are more common in the cervical and axillary regions. They are unusual in abdominal and pancreas location.
Its incidence is estimated at around 1:100,000 and 1:20,000 admissions in adults and in children. Despite the long recognition of this disease, its origin classification and pathology remain controversial. The highest incidence is between the third and fourth decades of life, with 75% of those diagnosed after ten years with a slight female predominance. Lymphangiomas are a major group of so-called vascular hamartomas, which result from a failure in the evolutionary development of the vascular system, including lymphatic and or arteries and veins. Diagnosis is made by biopsy of suspicious nodules, other imaging techniques such as CT, MRI, and ultrasound. The complete surgical excision is the ideal treatment for mesenteric lymphangionma. We report our experience with a rare case of mesenteric lymphangioma in a middle-aged male.
Case report:
A 43-years old man was admitted to our institution with left upper quadrant pain from two months.He presented with a good general condition, acyanosis and was afebrile, hydrated, normotensive BP 110/80 mmHg, HR - 96 beats/per min arrhythmic with symmetrical heart sound without murmur. SpO2 was 96%, both lungs with alveolar sounds, and there was no peripheral edema. His abdomen had painfulness to superficial and deep palpation. Chest X-ray showed no abnormality, lung field was clear and sinuses sharp. Computed tomography of the abdomen revealed a +2-(-8) HU hypodense mass of cystic aspect measuring 6.9x4.0x13.4 cm without contrast. Histopathologic examination confirmed a mesenteric cyst/lymphangioma. The patient was discharged without intercurrences.

Biography:
Coming Soon..
Abstract:
Coming Soon..
- Clinical Trails and Clinical Research
Location: Sydney, Australia
Session Introduction
Ladan Khodaparast
University of Leuven, Belgium
Title: Multi-targeted proteostatic collapse as an antimicrobial strategy against multiresistant Escherichia coli

Biography:
Ladan has completed her PhD in May 2017 from KU Leuven from department of Immunology and Microbiology and she currently works at the Faculty of Medicine, Switch Laboratory VIBâ€KU Leuven Centre for Brain & Disease Research Department of Cellular and Molecular Medicine, University of Leuven. Based on the aggregation propensity of proteins, short-stretch peptides were designed that induce specific aggregation of​ bacterial proteins resulting in bacterial death. The aim of her project is to evaluate the possible toxicity and efficacy of these peptides in vitro and in vivo. Ladan has published more than 8 papers in reputed journals.
Abstract:
This is a novel designer antibiotics paradigm that exploits protein aggregation to kill pathogenic E. coli by widespread proteostatic collapse. In order to induce multi-targeted protein aggregation, we designed P2, a synthetic peptide containing a short aggregation-nucleating sequence that is highly redundant in the E. coli proteome. P2 is readily internalized by E. coli, inducing rapid formation of large polar inclusions resulting from co-aggregation between P2 with bacterial proteins containing similar aggregation prone sequences, resulting in a lethal aggregation cascade involving over 300 proteins connected through a network of associated APRs. P2 is active against clinical isolates that are resistant to multiple antibiotics and is effective in reducing bacterial load in bladder infection in mouse. Our results indicate slow development of resistance, suggesting that aggregation of redundant APRs constitutes a tight proteostatic deadlock. Exploiting this finding could be useful as a novel therapeutic approach against drug-resistant bacteria.
Tiffany L Gould
University of Newcastle, Australia
Title: VTE prophylaxis in Acute General Surgical Patients, A local Audit

Biography:
Tiffany completed a Bachelor of Medicine from the Unviversity of Newcastle, awarded with Distinction in 2015. She has completed further studies in Advanced Surgical Anatomy, as well as a Diploma of Science and a Master of Traumatology awarded with Distinction in 2017. Tiffany is works as a Clinical Teaching Fellow with the University of Newcastle, a surgical registrar in Hunter New England Health and has commenced a research higher degree in the field of Colorectal Surgery and Preventative Medicine.
Abstract:
In 2008 a report found venous thromboembolism (VTE) represented 7% of all deaths in Australian hospitals and had a higher mortality than bowel or breast cancer (1). VTE cost an estimated 1.72 billion dollars with an additional 11.97-27.31 billion dollars value of lost wellbeing (1). In surgical patients, without contraindications, Hunter New England guidelines recommend 20mg of Enoxaparin given 2 hours prior to surgery for moderate risk patients and 40mg Enoxaparin 12 hours prior to surgery for high risk patients for the prevention of VTE (2) (3).
METHODS:
John Hunter Hospital electronic record data was audited over a three month period during which 339 patients underwent an operation under the care of AGSU (Acute General Surgical Unit). After application of predetermined exclusion criteria 254 patients were included for assessment. Risk stratification and timing intervals were defined as per local guideline.
Primary outcomes assessed:
- Enoxaparin use preoperatively
- Enoxaparin use postoperatively (within 24hrs)
-
Use of Enoxaparin in accordance with risk levels;
- High risk
- Low/Medium risk
-
Administration of Enoxaparin in accordance with recommended timing intervals pre-operatively according to risk.
- >2hrs Low/Medium
- >12hrs High
RESULTS:
A total of 35% of patients received pre-operative prophylaxis, 23.6% of which received the correct dosing according to risk. Of patients receiving pre-operative prophylaxis 91% received pharmacotherapy at the recommended timing interval according to risk.
Overall 31% of patients received post-operative prophylaxis and a total of 27% of patients received both pre-operative and post-operative prophylaxis. Of the total sample population 62% of patients did have Enoxaparin charted pre-operatively however in 44% of these patients pharmacotherapy was withheld; of these patients only 15% had documented reasons why.
Laleh Khodaparast
University of Leuven, Belgium
Title: Characterisation of the biofilm phenotype of methicillin- susceptible and resistant Staphylococcus aureus in UZ hospital Leuven

Biography:
Laleh Khodaparast has completed her PhD in May 2017 from KU Leuven, Department of Microbiology and Immunology. Laleh Khodaparast is postdoctorate at the Faculty of Medicine, Switch Laboratory VIBâ€KU Leuven Center for Brain & Disease Research Department of Cellular and Molecular Medicine, University of Leuven. She is currently working on a new antibacterial strategy which uses synthetic peptides to combat gram-negative bacteria. Laleh has published more than 8 papers in reputed journals such as Nature communication (first author) and science and has been serving as an editorial board member of repute.
Abstract:
The ability of antibiotic-resistant bacteria to form biofilms makes them both more virulent and more difficult to treat. There are several virulence factors that help them to express this behaviour.
Here, the biofilm phenotype of a collection of clinical isolates of S. aureus that were collected from the patients in UZ-hospital-Leuven in Belgium was investigated. The biofilm-forming behaviour and phenotypic results were compared between antibiotic-resistant and antibiotic-sensitive MRSA and MSSA strains, which indicated a common protein-dependent biofilm in both strains, especially the MRSA strains. This suggests that cell wall-anchored proteins are important factors and mostly cause cell adherence.
- Case Reports on Obstetrics & Gynecology
Location: Sydney, Australia
Session Introduction
Samantha Quennie
Nicanor Reyes Memorial Foundation Medical Center, Philippines
Title: Placenta percreta induced third trimester uterine rupture in an Unscarred uterus: A diagnostic dilemma

Biography:
Samantha Quennie Wanasen-Razon has completed her Degree of Medicine at the age of 24 years from Far Eastern University- Nicanor Reyes Memorial Foundation Medical Center. She is currently a Third year Obstetrics and Gynecology Resident in the said institution.
Abstract:
Cases of uterine rupture induced by placenta percreta in an unscarred uterus are rare. This is a case of 30-year-old, Gravida 2 Para 1 (1001) Pregnancy Uterine 31 Weeks and 2 days age of gestation with persistent generalized abdominal pain found out to have uterine rupture secondary to placenta percreta. This paper aims to discuss the differential diagnoses for cases of third trimester abdominal pain, the appropriate diagnostic modalities and the best management for such case. Uterine rupture should be considered in the differential diagnosis in all pregnant women who present with acute abdomen even if there are no risk factors. Exploratory laparotomy was done to investigate the cause of the patient’s severe abdominal pain on top of intrauterine fetal bradycardia. During the procedure, uterine rupture with massive bleeding was detected; therefore, subtotal abdominal hysterectomy was performed. The patient was discharged without any complications. Pathological analysis of the uterine specimen revealed placenta percreta to be the cause of the rupture.
KEY WORDS: Placenta Accreta, Increta, Percreta; Abruptio Placentae; Uterine Rupture; Preterm Labor; Total Abdominal Hysterectomy

















